 Thoracic Outlet Syndrome:
Thoracic Outlet Syndrome:
Why Do We Take a Pulse When the Problem is Neurologic?
Structures Involved in Thoracic Outlet Syndrome
Thoracic Outlet Syndrome (TOS) is a term to describe a compression disorder. There are four areas that are potentially problematic: thoracic inlet, scalene triangle, coracopectoral loop, and pectoralis minor loop. Within these areas there are three structures that could potentially be compressed: brachial plexus, subclavian artery, and subclavian vein. Causes of TOS can be rather diverse. Trauma, repetitive activities, poor posture, and anatomic anomalies can contribute. TOS is classification by the structure involved:
- Neurogenic TOS – most common type and characterized by compression of the brachial plexus
- Vascular TOS – occurs when the subclavian artery or subclavian vein are compressed
Of course, signs and symptoms of TOS depend on the structure compressed. This image describes the possible presentation(s): 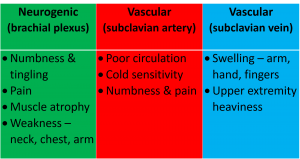
Typically when clinical tests are discussed, the techniques used for the rendering of a diagnosis are explained and then the supporting metrics are referenced. In the case of TOS tests, the techniques used for diagnostic purposes have some inherent problems. So it makes sense to discuss this first. Historically, thoracic outlet tests have only looked at circulation, i.e. using the radial pulse as the indicator of a positive or negative test. If the pulse quality was diminished/absent in the test position, the test was deemed positive. But which is it, diminished or absent? If diminished, by how much? This makes a difference in the interpretation and in part, explains the wide variability of the metrics. Yet, vascular compression is significantly less common (only 4-6% of TOS diagnoses) than neural compression. Some researchers (Lindgre, 2010; Plews & Delinger, 1998) have differentiated pulse diminution from pain/paresthesias as the barometer for a positive test. This is helpful not only regarding sensitivity and specificity but it is also may identify the structure involved in the pathology, i.e. neural vs vascular. Fortunately, the work of Lindgre (2010) reported data using the clustering of tests to assist in a diagnosis. Individual test data, as well as the clustering of tests, are revealed in the following chart.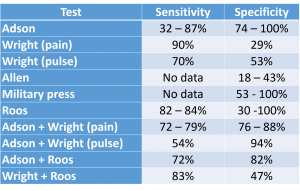
There is one more pearl worth sharing to help the clinician remember the procedure for each of the TOS tests. The pearl is “the rule of the thumb,” i.e. the head rotation always follows the direction of the thumb. This will be helpful in distinguishing the direction to which the head should be turned in testing. This will become apparent as the steps of each test are revealed. So let’s get to the actual performance of five TOS tests: Adson, Wright (hyperabduction), Allen, Military press (Eden), and Roos (EAST).
Adson Test
Adson test is performed with the shoulder stabilized. The clinician takes the radial pulse as a baseline. Attention should be paid to the quality of the pulse as well as the rate. This will be important to ascertain if the pulse quality decreased. The UE is then passively moved into abduction, extension, and external rotation (ER). Next, the head is rotated toward involved side. Remember, the thumb is facing ipsilaterally, so you’re going to rotate ipsilaterally. Have the client take a deep breath to engage the scalene muscles and hold it. Retake the pulse. A positive test is the reproduction of symptoms or an absent or diminished pulse.
 Wright Test, AKA Hyperabduction Test
Wright Test, AKA Hyperabduction Test
This test also begins by taking the radial pulse with the arm at the side. Once the pulse is obtained, the arm is passively elevated overhead, and have the client takes a big, deep breath. Note, there is no head rotation in this test. This is consistent with the “rule of the thumb” – thumb is directly overhead so the head stays in neutral with no rotation. Care should be taken to bring the arm overhead with ER to avoid the possibility of creating impingement (Neer test). The Wright test has been suggested to incriminate the tissues in the coracopectoralis minor loop. When pulse is the diagnostic characteristic, sensitivity is 70% and specificity is 53%. However, when pain is the characteristic, sensitivity is 90% and specificity is 29%. In either situation, the Wright test is a better screening tool than a diagnostic tool. 
Allen Test
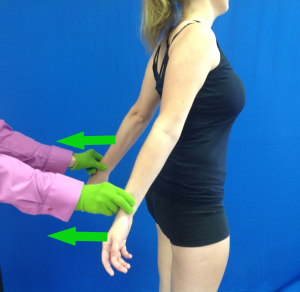
Once again, the Allen test begins with the taking of the radial pulse. In sitting, stabilize the trunk and passively take the UE into 90° of shoulder abduction with 90° of elbow flexion. Ask the patient to turn the head away (remember, thumb is facing contralateral), take a deep breath and hold it. Reproduction of pain or diminished/absent pulse suggests tissue compressed by the pectoralis minor muscle.
 Military Press Test
Military Press Test
The military press test, also known as the Eden test, detects tissue compressed at the costoclavicular region (between 1st rib and clavicle). In this test, the radial pulses are obtained bilaterally with the UE’s at the side. In either sitting or standing, the shoulders are retracted into extension and abduction with the neck in extension (exaggerated military posture). Reproduction of pain or diminished/absent pulse is a positive test.
Roos Test
The Roos test, also known as the EAST (Elevated Arms Stress Test), looks like you are performing a party dance, but it has some of the best statistics of the TOS tests. In sitting with the UE’s at 90° of shoulder abduction, ER, and elbow flexion, the client is instructed to open and close his/her hands for 3-minutes. A positive test is paresthesias of the hands, heaviness of the hands, and/or a color change. One should also observe the symmetry and/or slowing of the opening and closing of the fist. This could also be interpreted as a positive test.
Clinical Interpretation
In summary, these 5 TOS tests have highly variable metrics that may be influenced by the symptom(s) used to determine is the test is positive or negative. Given that brachial plexus compression is much more common, paresthesia and numbness should be expected to occur with greater frequency. However, no diagnosis should be based on the outcome of one test. The clustering of tests and the presentation of other signs, symptom, and mechanisms of injury should be considered.
More cutting-edge orthopedic information can be found in iOrtho+ Premium Mobile App. Subscribe for the low annual rate of only $9.99. If you prefer to just try iOrtho+ Premium for 1 month, you can do so for only $1.99 Please visit https://iortho.xyz/ Prior blog posts are also available at https://iortho.xyz/
- Adson AW, Coffey JR. Cervical rib: a method of anterior approach for relief of symptoms by division of the scalenus anticus, Annals Surgery 1927;85:839-857
- Gillard J, Perez-Cousin M, Hachulla E, Remy J, Hurtevent JF, Vinckier L, Thevenon A, Duquesnoy B. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint Bone Spine. 2001 Oct; 68(5): 416-424
- Gulick DT. iOrtho+ Web App. DTG Enterprises LLC. 2024
- Gulick, DT. OrthoNotes, 5th FA Davis Publishing, Philadelphia. 2023
- Howard M, Lee C, Dellon AL. Documentation of brachial plexus compression utilizing provocative neurosensory & muscle testing. Journal Reconstructive Microsurgery. 2003;19(5):303-312
- Lee AD, Agarwal S, Sadhu D. Doppler Adson’s test: predictor of outcome of surgery in non-specific thoracic outlet syndrome. World Journal of Surgery. 2006;30(3):291-292
- Lindgre K-A. Thoracic outlet. International Musculoskeletal Medicine. 2010;32(1):17-24
- Marx RG, Bombardier C, Wright JC. What do we know about the reliability & validity of physical examination tests used to examine the upper extremity? Journal of Hand Surgery. 1999;24A:185-193
- Plews MC, Delinger M. The false-positive rate of thoracic outlet syndrome shoulder maneuvers in healthy patients. Academy Emergency Medicine. 1998;5(4):337-342
- Rayan GM, Jensen C. Thoracic outlet syndrome: provocative examination maneuvers in a typical population. Journal of Shoulder & Elbow Surgery. 1995;4(2):113-117
- Roos DB. Historical perspectives & anatomical considerations. Thoracic outlet syndrome. Seminars Thoracic Cardiovascular Surgery. 1996;8:183-189
- Wright IS: The neurovascular syndrome produced by hyperabduction of the arms, American Heart Journal. 1945; 29:1-19

