

Putting “Special Tests” in Perspective
I recently read a manuscript published in JOSPT (May 2020, Volume 20, Number 5) by Dr. Paul Salamh and Dr. Jeremy Lewis. The manuscript was entitled, “It Is Time to Put Special Tests for Rotator Cuff-Related Shoulder Pain out to Pasture.” The authors called to light that there are over 70 clinical tests for the shoulder labrum, rotator cuff, acromioclavicular joint, and biceps tendon. They appropriately questioned the validity of these tests. They spoke to the examination of 123 people with shoulder discomfort. Imaging of both shoulders revealed as many abnormalities in the pain-free shoulder as there were in the symptomatic shoulder. This is not a surprise. We have seen similar data when exploring radiographs of the low back. Abnormalities are often present on radiographs that are not consistent with the clinical presentation. We also see individuals with very severe osteoarthritic changes who you wonder how they are able to walk at all while those with what appear to be limited osseous changes are in severe pain. So they challenged the ability of imaging to be the “gold standard” for comparison for clinical tests for the shoulder. The authors raise some important questions.

 I have been teaching and writing about clinical tests for a couple decades. I have taken an evidence-based approach. In doing so, I have had to try to reconcile why a test can be studied by a variety of researchers with such highly variable results.
I have been teaching and writing about clinical tests for a couple decades. I have taken an evidence-based approach. In doing so, I have had to try to reconcile why a test can be studied by a variety of researchers with such highly variable results.
Salamh and Lewis cite inability of the empty-can and full-can tests to isolate the supraspinatus. They are correct. These tests engage 8-9 muscles each. The data below is a summary of some of the statistical data for these two tests.
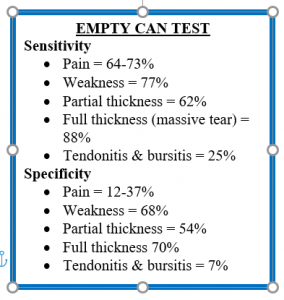
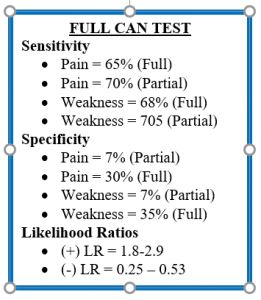
So what does a clinician do with this data? Perhaps the first question should be “how does such variable data exist?” Having read thousands (yes, I said thousands) of articles about special tests to develop the mobile app iOrtho+, I can tell you that what I have observed is the variability of the standardization of the test performance and the inconsistency in the criteria for a positive test. Look at the difference in the metrics for empty can test specificity. If the criteria for a positive test is pain, specificity is 12-37% while if the criteria for a positive test is weakness, specificity is 68%. In addition, with the plethora of anatomic structures incriminated by these tests, it is imperative the clinician ask the patient to “put 1-finger on the place you feel discomfort this the test.” This allows the clinician to target the symptomatic tissue.
However, one should consider two of Magid’s 10 radiographic commandments:
In other words, using only one perspective, whether that be a radiograph, a clinical test, or a patient symptom, is of little value. As clinicians we need to clutter the signs and symptoms, range of motion assessment, manual muscle testing, and clinical tests to accurately arrive at a diagnosis. The use of clinical questionnaires like the SPADI (Shoulder Pain and Disability Index), Penn Shoulder Score, and the Quick DASH (Disabilities of the Arm, Shoulder, and Hand) for the shoulder can assist in appreciating the dysfunction as opposed to just pain. This will allow us to “treat the patient not the radiograph/clinical test.”
So, do special tests have value? Of course, they do. Is some of it limited? Yes, without a doubt. Some the metrics demonstrate this fact. However, there is evolving literature by researchers such as Kai et al (2015) who studied the empty can and full can tests in various positions using electromyography. They performed isometrically with the shoulder elevated at 45° and 90° in the sagittal, scapular, and coronal planes, in the thumb-up or thumb-down positions. They reported activation of the rotator cuff muscles are influenced by position and plane of elevation. The supraspinatus and subscapularis activity were greater during the thumb-down test and in the scapular and coronal planes at 90°. More work needs to be done in this area for the shoulder, as well as other joints, to enhance our ability to put more stock in the outcomes of clinical tests. Thus, I disagree with Salamh and Lewis (2020) that they should eliminate special tests from our physical examination. We simply need to put them in perspective. Just like we recognize the margin of error of goniometric measures, we need to appreciate the variable contribution of some special tests. Clinicians need to do their best to stay in touch with the literature. OR….. even better yet, contribute to it!
For more cutting edge orthopedic information or iOrtho+ Premium Mobile App, please visit the learning modules at https://iortho.xyz/
- Dutton M. Orthopedic examination, evaluation & intervention, New York, McGraw Hill, 2004
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC, 2020
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia, 2018
- Itoi E, Kido T, Sano A, Urayama M, Sato K. Which is more useful, the full can test or the empty can test in detecting the torn supraspinatus tendon. American Journal of Sports Medicine. 1999;27(1):65-68
- Kai Y, Gotoh M, Madokoro K, et al. Electromyographic study of rotator cuff muscle activity during full and empty can tests. Asia Pacific Journal of Sports Medical & Arthroscopic Rehabilitation. 2015 Jan; 2(1): 36–41.
- Magid D. Magid’s 10 Radiographic Commandments. http://teamrads.com/index.php/radiology-elective/lecture-handouts/magid-s-10-radiographic-commandments
- Ostor AJ, Richards CA, Prevost AT, Hazleman BL, Speed CA. Interrater reproducibility of clinical tests for rotator cuff lesions. Annals Rheumatic Disease. 2004;63:1288-1292
- Sgroi M, Loitsch T, Reichel H, Kappe T. Diagnostic value of clinical tests for supraspinatus tendon tears. Arthroscopy. 2018;34(8):2326-2333
- Somerville LE, Willits K, Johnson AM, Litchfield R, LeBel M-E,Moro J, et al. Clinical assessment of physical examination maneuvers for rotator cuff lesions. American Journal of Sports Medicine. 2014;42:1911-1919
