 Is it broken?
Is it broken?
That is often the first question asked about an ankle injury. Unless you have x-ray eyes, you don’t have that immediate answer. Yes, a radiograph is the answer. However, there are clinical tests that can help you determine if a radiograph is really necessary. In 1992, Stiell et al conducted a pilot with 155 adults and a main study with 750 adults. All experienced acute ankle injuries. They identified the clinical variables capable of predicting fractures and/or the need for radiographs. What they found was that all 70 malleolar fracture identified in 689 ankle radiographs identified pain near the malleoli, were over 55 years of age, had local tenderness on the posterior edge or tip of the malleoli, or were unable to bear weight immediately/in the emergency room. Using these rules, the sensitivity was 100% and specificity was 40%. Equally impressive is the fact that using these “rules” would allow for a reduction of 36% of radiographs ordered. Further studies fine-tuned these “rules” to become the Ottawa Ankle and Ottawa Foot Rules.
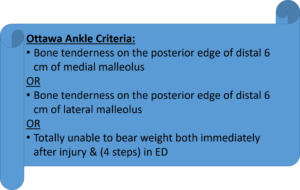
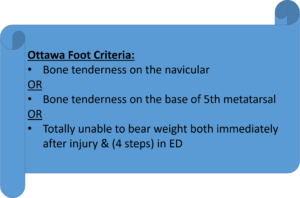


Interpretation is if ANY of the criteria are positive, a radiographic series is warranted. Both of these sets of rules have been studied extensively. They have been validated for both adults and children. These data are displayed below:
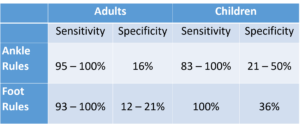
As per the statistical data, one can see from the low specificity, the Ottawa Rules are not intended to be diagnostic of a fracture. The high sensitivity tells us they are designed be a reliable screening tool to determine if a radiograph is needed. Fortunately, radiographs have a specificity of 88% – making them a strong diagnostic tool.
Metatarsal Load Test
Another bone commonly fractured is the 5th metatarsal. This injury is known as a Jones fracture. The metatarsal load test is used to evaluate the potential of this injury. The clinician grasps the metatarsal distal aspect of the 5th metatarsal and applies a longitudinal load. A positive test is reproduction of pain along the shaft of the 5th metatarsal.
Bone Stress Injuries
Not all bone injuries are displaced fractures. Bone stress injuries (BSI) are the inability of a bone to withstand repetitive loading. Nye et al (2016) developed an algorithm to improve diagnostic accuracy of suspected bone injuries. These include Risk Factors, Symptoms, and Examination elements.
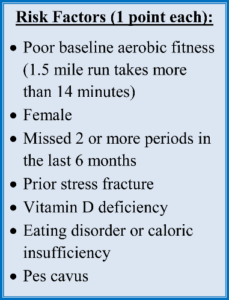
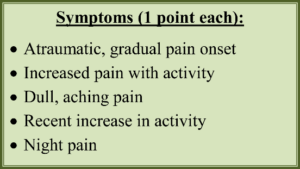
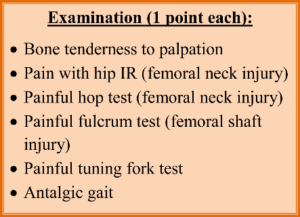
High risk structures include femoral neck, anterior tibia, medial malleolus, navicular, talus, proximal 2nd and 5th metatarsals, patella, and toe sesamoids. Interpretation of the BSI score is as follows: a score ≥ 4 and at least 1 examination finding. If this criteria is achieved, radiographs should be obtained and activity/weight bearing should be restricted.
Other techniques for stress fractures include the bump test, tuning fork, and therapeutic ultrasound.
Bump Test
The Bump test is done in a non-weight bearing position. With the ankle in neutral, the lower leg is stabilized and the clinician applies a firm, controlled, longitudinal force (bump) with the thenar eminence to the patient’s heel. If a fracture is present, the reverberating force will produce the pain.
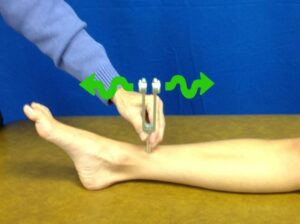 Tuning Fork
Tuning Fork
The use of a 256 Hz tuning fork and therapeutic ultrasound function in a similar way for discerning the presence of a fracture. The vibration over the periosteum of a stressed bone has been shown to produce pain in the region of the stress fracture. The use of a vibrating tuning fork over the area of discomfort has been reported to have limited diagnostic value (specificity = 67%) and modest screening value (sensitivity = 75%).
Ultrasound
A 1-MHz frequency ultrasound transducer at 2.0 w/cm2 for 30 seconds over the region of the suspected stress fracture can be used to reproduce pain. This would be deemed a positive test. Again this technique a specificity of 67% but a (+) predictive value of 99%. Sensitivity is 82% with a (-) predictive value of 13%.
In summary, we have a variety of tools to assess fractures and stress injuries. These should be used in conjunction with the mechanism of injury, the risk factors of the individual (history of eating disorders, menstrual irregularities, prior stress fracture), lower extremity malalignment, and recent changes in training techniques/intensities. Together these factors will help the clinician determine an appropriate course of action.
Please visit https://iortho.xyz/
- Auleley GR, Kerboull L, Durieux P, Courpied JP, Ravaud P. Validation of the Ottawa rules in France: A study in the surgical emergency departments of a teaching hospital. Annals Emergency Medicine 1998; 32:14-18
- Auletta AG, Conway WF, Hayes WF, Guisto DF, Gervin AS. Indications for radiography in patients with acute ankle injuries: Role of the physical examination. American Journal Radiology 1991; 157:789-791
- Beck B. Can therapeutic ultrasound accurately detect bone stress injuries in athletes? Clinical Journal of Sports Medicine. 2013;23(3):241-242
- Burrus MT, Werner BC, Starman JS, Gwathmey FW, Carson EW, Wilder RP, Diduch DR. Chronic leg pain in athletes. American Journal of Sports Medicine. 2014;43(6):1538-1547
- Cotton FJ: Fractures & Fracture-Dislocations, Philadelphia, 1910, WB Saunders
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC. 2025
- Gulick, DT. OrthoNotes, 5th FA Davis Publishing, Philadelphia. 2023
- Kerr L, Kelly AM, Grant J, et al. Failed validation of a clinical decision rule for the use of radiography in acute ankle injury. New Zealand Medical Journal 1994; 107:294-295
- Lesho EP. Can tuning forks replace bone scans for identification of tibial stress fractures? Military Medicine. 1997;162:802-803
- Lindenfeld T, Parikh S: Clinical tip: heel-thump test for syndesmotic ankle sprain, Foot Ankle International 2005;26:406-408
- Magee D. Orthopedic Physical Assessment. 5th ed. Philadelphia, PA: WB Saunders Company; 2008.
- Nye NS, Covey CJ, Sheldon L, Webber B, Pawlak M, Boden B, Beutler A. Improving diagnostic accuracy and efficiency of suspected bone stress injuries: Algorithm and clinical prediction rule. Sports Health. 2016;May-June;8(3):278-283
- Stiell I, Wells G, Laupacis A, et al for the Multicentre Ankle Rule Study Group. Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle injuries: British Medical Journal 1995; 311:594-597
- Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Annuals Emergency Medicine 1992; 21:384-390
- Stiell IG, McKnight RD, Greenberg GH et al. Ottawa Foot & Ankle Rules. Journal American Medical Association. 1994;271:827
