

Arches of the Foot: Challenge of Mobility & Stability
Do you count your steps each day? With the popularity of wearable devices to monitor our activity, many people have accepted the challenge to count their steps daily. Various organizations have quantified the number of steps into categories:
- Low active is 5,000 to 7,499 steps per day
- Somewhat active is 7,500 to 9,999 steps per day
- Active is more than 10,000 steps per day.
- Highly active is more than 12,500.
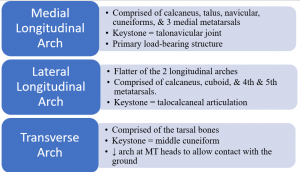
The feet are where each of these steps begin. There are 3 arches of the foot that provide both mobility and stability to ambulate. The 3 arches include:
The function of the arches of the foot include:
-
-
- Weight distribution
- Adapt to conversion of foot to rigid lever
- Dampens shock of weight-bearing
- Adapt to changes in support surface
-
This dichotomy of mobility and stability of the foot set it up for a variety of injuries. There are at least 3 tests that can be used to assess varying types of mobility (or lack of mobility) of the ankle and foot. The navicular drop, Coleman block, and windlass test will be discussed.
 The navicular drop test assesses midfoot mobility. The test has two steps: non-weight bearing and weight bearing. Step #1: Sitting with the foot on the floor, the clinician measures the distance from the navicular tuberosity to the floor. Step #2: Standing with weight equally distributed on both feet, the clinician measures the distance between the same anatomic structures.
The navicular drop test assesses midfoot mobility. The test has two steps: non-weight bearing and weight bearing. Step #1: Sitting with the foot on the floor, the clinician measures the distance from the navicular tuberosity to the floor. Step #2: Standing with weight equally distributed on both feet, the clinician measures the distance between the same anatomic structures.
It is normal for the navicular to drop in weight bearing. A drop of 6 – 8 mm is considered normal and 10 – 15 mm is considered abnormal. In addition, the navicular should drop the same amount in each foot. Excessive navicular drop has been associated with shin splints, medial tibial stress fractures, and patellofemoral tracking abnormalities. There is no published data on sensitivity or specificity of this test but reliability of the measure has been reported to range from 0.57 to 0.78.
The Coleman block test assesses hindfoot mobility as it relates to a plantarflexed first ray versus a tight tibialis posterior muscle. While standing (#1), the clinician measures the alignment of the hindfoot, i.e. how much rearfoot varus or valgus. Then, the client is asked to stand (#2) with on a 2 cm block under the lateral aspect of the foot (some suggest placing the block under the entire foot with the exception of the first ray- #3).
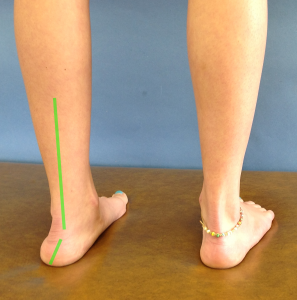
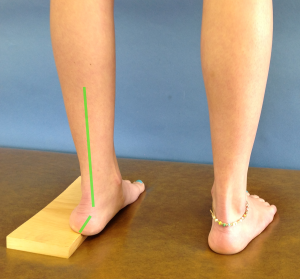
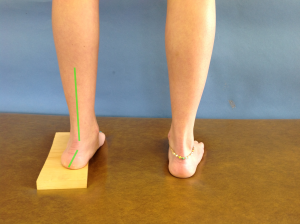
The response of the hindfoot (varus/valgus) to standing on the block is observed. If the hindfoot has less varus (moves towards valgus) when standing on the block, the hindfoot has adequate flexible and the problem is a plantarflexed first ray. Whereas, if the hindfoot does not have less varus, the problem is limited hindfoot mobility attributed to tibialis posterior muscle tightness. Although there is no statistical data on this test, the positioning and biomechanical process makes sense.

 The Windlass test is used to assess the plantarfascia tension. There is a weight-bearing (WB) and non-weight-bearing (NWB) component to this test also. In NWB, the ankle is stabilized in neutral and the great toe is dorsiflexed. In WB, with equal weight on both feet, the great toe is again dorsiflexed. Pain along medial longitudinal arch would be a positive test. The statistics for this test reveals it is an exceptional diagnostic tool (sensitivity = 13.6 – 31.8%; specificity = 100%) with high reliability (0.96 – 0.99).
The Windlass test is used to assess the plantarfascia tension. There is a weight-bearing (WB) and non-weight-bearing (NWB) component to this test also. In NWB, the ankle is stabilized in neutral and the great toe is dorsiflexed. In WB, with equal weight on both feet, the great toe is again dorsiflexed. Pain along medial longitudinal arch would be a positive test. The statistics for this test reveals it is an exceptional diagnostic tool (sensitivity = 13.6 – 31.8%; specificity = 100%) with high reliability (0.96 – 0.99).
These 3 tests provide the clinician with information about the medial longitudinal arch and the structures that support it. Based on the results of these tests, the patient might benefit from stretching, strengthening, or orthotic support.
For more cutting edge orthopedic information, subscribe to iOrtho+ Premium Mobile Web App, at https://iortho.xyz/
- Alshami AM, Babri AS, Souvlis T, Coppieters MW. Biomechanical evaluation of two clinical tests for plantar heel pain: the dorsiflexion-eversion test for tarsal tunnel syndrome and the windlass test for plantar fasciitis. Foot & Ankle International. 2007 Apr;28(4):499-505
- Deben SE, Pomeroy GC. Subtle cavus foot: Diagnosis and management. Journal of the American Academy of Orthopaedic Surgeons. 2014 Aug;22(8):512-520.
- DeGarceau D, Dean D, Reduejo SM. Thordarson DB. The association between diagnosis of plantarfascitis & Windlass test results. Foot & Ankle International. March 2003;24(3):251-255
- Deng J, Joseph R, Wong CK. Reliability and validity of the sit-to-stand navicular drop test: Do static measures of navicular height relate to the dynamic navicular motion during gait? Journal of Student Physical Therapy Research 2010;2:21-28.
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC. 2020
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia. 2018
- Kim JY, Keun Hwang S, Tai Lee K, Won Young K, Seon Jung J. A simpler device for measuring the mobility of the first ray of the foot. Foot and Ankle International. 2008 Feb;29(2):213-218.
- Loudon JK, Jenkins W, Loudon KL: The relationships between static posture and ACL injury in female athletes, J Orthop Sports Phys Ther. 1996; 24:91-97
- Mueller MJ, Host JV, Norton BJ: Navicular drop as a composite measure of excessive pronation, J Am Pod Med Assoc. 1993; 83:198-202
- Myerson MS, Badekas A. Hypermobility of the first ray. Foot and Ankle Clinics. 2000 Sept;5(3):469-484
- Picciano AM, Rowlando MS, Worrell T: Reliability of open and closed kinetic chain subtalar joint neutral positions and navicular drop test, J Orthop Sports Phys Ther. 1993; 18:553-558
- Shultz SJ, Nguyen AD, Windley TC, Kulas AS, Botic TL, Beynnon BD. Intratester and intertester reliability of clinical measures of lower extremity anatomic characteristics: Implications for multicenter studies. Clin J Sport Med 2006;16:155-161.
- Sell KE, Verity TM, Worrell TW, Pease BJ, Wigglesworth J. Two measurement techniques for assessing subtalar joint position: a reliability study. J Orthop Sports Phys Ther 1994;19:162-168.
- Shrader JA, Poporich JM, Gracey GC et al: Navicular drop measurement in people with rheumatoid arthritis: interrater and intrarater reliability, Phys Ther. 2005; 85:656-664.
