BLOOD PRESSURE: It’s called a “Vital Sign” for a reason
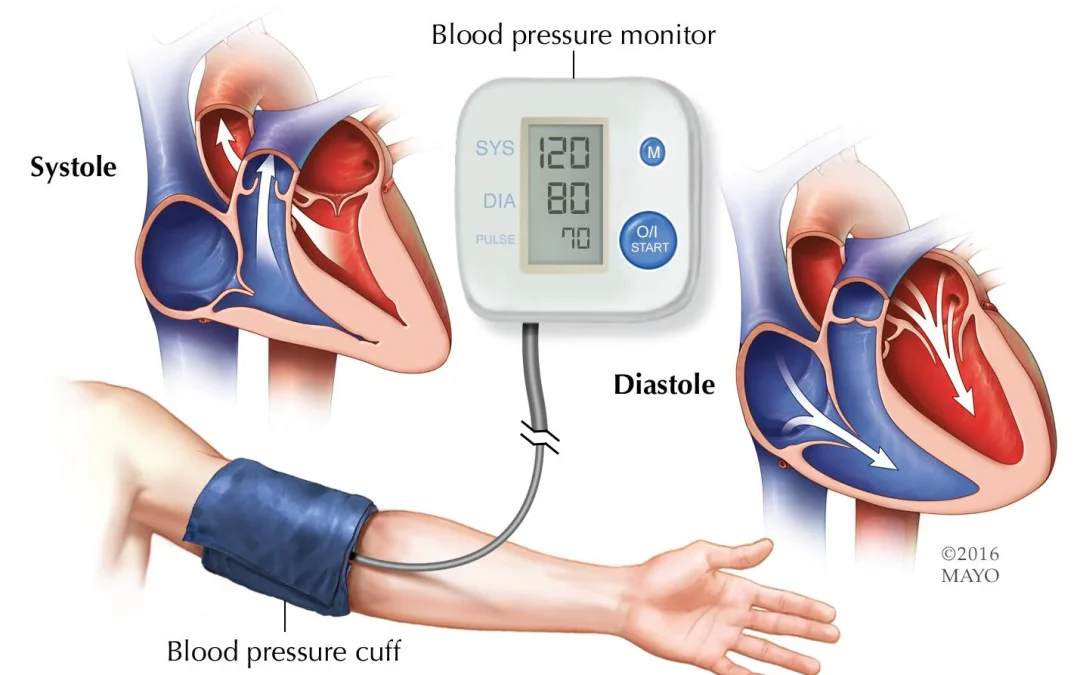
Reliable and accurate blood pressure (BP) measurements are essential for proper diagnosis and treatment of medical conditions. There is a reason BP is known as a “vital sign.” It has been estimated that a measurement error of 5 mm Hg can impact a hypertension diagnoses in 84 million people worldwide (Journal of Hypertension). Likewise, inappropriate measures can negatively influence 20%-45% of cases (Lancet Commission of Hypertension Group). Drs Michael Rakotz and Gregory Wozniak reported that despite efforts to enhance awareness of these issues, the problem persists.
The adverse effects of inaccurate measures extend beyond a hypertensive diagnosis. Inappropriate treatment(s) can result in prescribing unnecessary or insufficient medications and lead to dangerous effects influencing the cardiovascular, renal, and/or visual systems. Furthermore, side effects or medication interactions can also result in negative outcomes. Misdiagnoses can have secondary ramifications such as increased cost, patient stress, and/or lost wages.
So how can we do better? Standardized techniques are available but if clinicians are not aware of them or don’t follow them, they are of little value. Let’s put the components into 4 categories.
- Patient related
- Procedurally related
- Equipment related
- Environmentally related
Patient related factors span a large variety of possibilities. Some patients have “white coat hypertension” which can temporarily raise BP. Likewise, recent physical activity, caffeine, nicotine, or alcohol ingestion can raise BP. Even a full bladder can elevate systolic pressure 10-15 mmHg. Attention should be given to positioning since sitting without back supported or having the legs crossed can impact readings.
Procedural factors relate to the way we perform the taking of BP. This may include a cuff placed over clothing or the arm not being placed at heart level. A study by Pickering (1993) demonstrated the impact of the arm position on BP measures.



When time constraints are present, clinicians may deflate the cuff too rapidly and fail to identify precise systolic and diastolic sounds/measures. Although the inflation rate has not been shown to have an influence on BP, very slow or very fast deflation rates can present a problem. Deflation rate ≤ 2mm Hg/sec can result in slightly higher diastolic BP (DBP). Whereas, deflation rates faster than 10 mm Hg/sec can result in the clinician missing critical Korotkoff sounds.

Equipment related factors include poorly calibrated or improperly charged electronic monitors. Selecting an incorrect cuff for the size of the patient can also produce incorrect readings. If the cuff is too small, the result could be a falsely high value. If the cuff is too large, the result could be a falsely low reading. The American Heart Association recommends the following cuff sizes to confirm an accurate BP assessment.
Finally, environmental factors may include very hot or very cold venue. For some individuals, very loud or busy environments can increase their stress levels which can impact their BP.
So all that being said, what is the correct/standardized procedure for correctly assessing BP? These are the parameters recommended by the American Heart Association.
- Don’t drink a caffeinated beverage or smoke during the 30 minutes before assessing BP
- Sit quietly for five minutes
- Sit in a chair with a back with feet on the floor
- Support the arm with the elbow is at heart level
- Size the cuff so the inflatable part of the cuff completely covers at least 80% of the upper arm
- Place the cuff on bare skin, not over a shirt
- Don’t talk during the measurement
- Deflate the cuff at a rate of 2 to 3 mm Hg/sec
 It’s a good idea to have your blood pressure measured in both arms at least once, since the reading in one arm (usually the right) may be higher than that of the left. In general, the arm-to-arm difference in systolic BP (SBP) should be 5 mm Hg or less. If the difference is consistently greater than 10 mm Hg between the two arms, this could be a sign of arterial plaque buildup. Furthermore, clinical decisions should not be made on a single BP measure. Serial measures should be performed over several days and different times of the day to identify pathology like hypertension (HTN). The following are the ranges for the stages of hypertension identified by the Mayo Clinic:
It’s a good idea to have your blood pressure measured in both arms at least once, since the reading in one arm (usually the right) may be higher than that of the left. In general, the arm-to-arm difference in systolic BP (SBP) should be 5 mm Hg or less. If the difference is consistently greater than 10 mm Hg between the two arms, this could be a sign of arterial plaque buildup. Furthermore, clinical decisions should not be made on a single BP measure. Serial measures should be performed over several days and different times of the day to identify pathology like hypertension (HTN). The following are the ranges for the stages of hypertension identified by the Mayo Clinic:
If working with the pediatric population, it is important to realize that normal BP for a child is lower than that of an adult. This range is influenced by both growth rate and gender. Below is a range to be considered for a child.
| Age Group | Boys – SBP | Boys – DBP | Girls – SBP | Girls – DBP |
| Infant | 72 – 104 | 37 – 56 | 72 – 104 | 37 – 56 |
| Toddler – 1 year | 86 – 101 | 41 – 54 | 85 – 102 | 42 – 58 |
| Toddler – 2 year | 89 – 104 | 44 – 58 | 89 – 106 | 48 – 62 |
| Pre-school – 3 year | 90 – 105 | 47 – 61 | 90 – 107 | 50 – 65 |
| Pre-school – 4 year | 92 – 107 | 50 – 64 | 92 – 108 | 53 – 67 |
| Pre-school – 5 year | 94 – 110 | 53 – 67 | 93 – 110 | 55 – 70 |
| School age – 6 year | 90 – 109 | 59 – 73 | 91 – 108 | 59 – 73 |
| School age – 7 year | 91 – 111 | 60 – 74 | 92 – 110 | 60 – 74 |
| School age – 8 year | 93 – 113 | 60 – 75 | 94 – 112 | 60 – 75 |
| School age – 9 year | 94 – 115 | 61 – 75 | 95 – 114 | 61 – 76 |
| School age – 10 year | 96 – 117 | 62 – 76 | 97 – 116 | 62 – 77 |
| School age – 11 year | 98 – 119 | 62 – 77 | 99 – 118 | 63 – 78 |
| School age – 12 year | 100 – 121 | 63 – 78 | 100 – 120 | 64 – 78 |
| Adolescent > 13 year | 102 – 124 | 64 – 80 | 102 – 121 | 64 – 79 |
In summary, BP is a “vital sign” and it needs to be performed in a standardized way to be reliable and valid. Failure to standardize the technique does not permit appropriate comparisons of serial measures. Clinical decisions made as a result of this measure depend on it being precise. So, please take the time to do it right!
More cutting-edge orthopedic information can be found in iOrtho+ Premium Mobile App. Subscribe for the low annual rate of only $9.99. If you prefer to just try iOrtho+ Premium for 1 month, you can do so for only $1.99 Please visit https://iortho.xyz/ Prior blog posts are also available at https://iortho.xyz/
- Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiology Clinician. 2013 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3639494/
- Pickering TG. Blood pressure variability and ambulatory monitoring. Curr Opin Nephrol Hypertens. 1993;2:380.
- American Heart Association. https://www.heart.org/-/media/files/health-topics/high-blood-pressure/tylenol-hbp/aha_toolkit_poster_final_102618.pdf
- Mayo Clinic https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/blood-pressure/art-20050982
- Flynn, Kaelber et al. 2017, National High Blood Pressure Education Program Working Group on High Blood Pressure in and Adolescents 2004