

Challenges of SI Tests: Part 2
In The Challenge of SI Testing – Part 1, eight sacroiliac joint (SIJ) tests were discussed. In The Challenge of SI Testing – Part 2, six additional tests will be discussed with statistical data regarding their clinical use. The six SIJ tests in Part 2 are:

The first 2 SIJ tests are performed in standing. The Flare Test begins by palpating the PSIS. The patient is asked to externally and internally rotate his/her hip with the foot on the ground. The clinician is looking for asymmetrical motion of the PSIS or a reproduction of symptoms to deem the test positive.
 The Weight Shift Test also is performed in standing while palpating bilateral PSIS. Again, the motion is compared when the patient shifts his/her weight from side to side. A positive test is reproduction of symptoms & increased/decreased mobility compared to the uninvolved side.
The Weight Shift Test also is performed in standing while palpating bilateral PSIS. Again, the motion is compared when the patient shifts his/her weight from side to side. A positive test is reproduction of symptoms & increased/decreased mobility compared to the uninvolved side.
The Resisted Abduction Test is performed in supine in 30 degrees of hip abduction. The clinician simply resists active hip abduction. Reproduction of pain over the SI joint is considered a positive test.
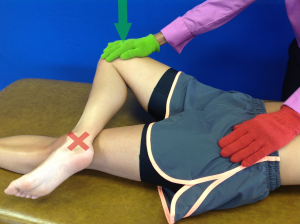
 For the Thigh Thrust or Posterior Shear (PoSh) Test, the clinician stands to the side of the patient supporting the hip in flexion, slight abduction, and ER. The clinician then applies a force through the long axis of the femur. Some clinicians opt to allow the knee on the testing leg to flex (unsupported) and use the other hand to stabilize the opposite pelvis with pressure on the contralateral ASIS. Reproduction of well localized pain over the ipsilateral gluteal region/SI joint is a positive test. This test has been reported to be negative in the presence of a lumbar herniated disc.
For the Thigh Thrust or Posterior Shear (PoSh) Test, the clinician stands to the side of the patient supporting the hip in flexion, slight abduction, and ER. The clinician then applies a force through the long axis of the femur. Some clinicians opt to allow the knee on the testing leg to flex (unsupported) and use the other hand to stabilize the opposite pelvis with pressure on the contralateral ASIS. Reproduction of well localized pain over the ipsilateral gluteal region/SI joint is a positive test. This test has been reported to be negative in the presence of a lumbar herniated disc.
Mennell Test is performed while sidelying on the involved side. The uninvolved lower extremity is extended and the involved hip/knee is flexed towards the chest. The clinician stands behind the patient and places 1 hand on the involved posterior pelvic crest/buttocks and other hand on involved knee in order to push involved leg into extension. A positive test is the reproduction of pain.
 FAbER Test uses the acronym FAbER to describe the position of the test: Flexion, Abduction, and External Rotation. In supine, the patient is placed in the FAbER position (also known as the figure-4 position). The contralateral pelvis is stabilized and overpressure is applied to the flexed knee. There are numerous structures that could potentially be incriminated. Pain assuming the position could be from the sartorius. Pain with over-pressure could be from the hip or the SI/LB. If the knee is more than 4 cm from surface, there may be a labrum problem.
FAbER Test uses the acronym FAbER to describe the position of the test: Flexion, Abduction, and External Rotation. In supine, the patient is placed in the FAbER position (also known as the figure-4 position). The contralateral pelvis is stabilized and overpressure is applied to the flexed knee. There are numerous structures that could potentially be incriminated. Pain assuming the position could be from the sartorius. Pain with over-pressure could be from the hip or the SI/LB. If the knee is more than 4 cm from surface, there may be a labrum problem.
For the 6 tests discussed in The Challenge of SI Testing – Part 2, the chart below displays the statistical data.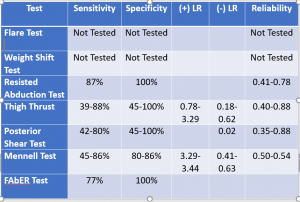
As stated in Part 1, Levangie (1999) reported individual test sensitivities were low (8%-44%), as were negative predictive values (28%-38%), for identifying the presence of innominate torsion in the Gillet, standing forward flexion, sitting forward flexion, and supine-to-sit tests. With the exception of the Gillet test (odds ratio = 4.57), combining tests did not improve performance characteristics.
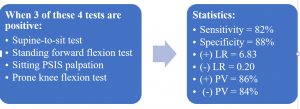
On the other hand, sometimes clustering of clinical tests can significantly increase the statistical value. A good example of this is the combination supine-to-sit, standing forward flexion, sitting PSIS palpation, and prone knee bend tests. When 3 of 4 tests are positive, the statistics are notably better:
In summary, the tests for the SIJ are very challenging. The ability to make an accurate diagnosis can be hampered by tests with high variability in their interpretation. The current ‘gold standard’ for diagnosing sacroiliac pathologies is a diagnostic nerve block. This is an injection of an anaesthetic inserted into the SIJ, under fluoroscopy guidance. However, there are risks in this technique. Thus, without high quality evidence for a multi-test regimen of sacroiliac joint tests, the challenge remains.
For more cutting edge orthopedic information subscribe to iOrtho+ Premium Mobile App, at https://iortho.xyz The annual subscription rate is only $1.99 per month or $9.99 per year
- Arab AM, Abdollahi I, Joghataei MT, et al. Inter- and intra-examiner reliability of single & composites of selected motion palpation & pain provocation tests of the sacroiliac joint. Manual Therapy. 2009;14:213-221
- Broadhurst NA, Bond MJ. Pain provocation tests for the assessment of sacroiliac joint dysfunction. Journal Spinal Disorder. 1998;11(4):341-345.
- Cibulka MT, Koldehoff R. Clinical usefulness of a cluster of sacroiliac joint tests in patients with and without low back pain. Journal Orthopedic & Sports Physical Therapy. 1999;29(2):83-92.
- Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history & physical examination in diagnosing sacroiliac joint pain. Spine. 1996;21(22):2594-2602
- Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrated short-term improvement with spinal manipulation. Spine. 2002;27:2835-2843
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC. 2020
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia. 2018
- Gutke A, Hansson ER, Zetherstrom G, Ostgaard HC. Posterior pelvic pain provocation test is negative in patients with lumbar herniated disc. European Spine Journal. 2009;18:1008-1012
- Helme RD. Measurement of flare responses in patients with pain. Clinical Experimental Neurology. 1987;24:201-205
- Hicks GE, Fritz JM, Delitto A, Mishock J. The reliability of clinical examination measures used for patients with suspected lumbar segmental instability. Archives of Physical Medicine 2003;84:1858-1864
- Kokmeyer D, van der Wuff P, Aufdemkampe G, Fickenscher T. Reliability of multi-test regimens with sacroiliac pain provocation tests. Journal Manipulative Physiological Therapeutics. 2002;25:42-48
- Laslett M, April C, McDonald B, Young S. Diagnosis of sacroiliac joint pain: validity of individual provocation tests & composites of tests. Manual Therapy. 2005;10:207-218
- Laslett M, Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine. 1994;19:1243-1249.
- Magee D. Orthopedic Physical Assessment. 5th ed. Philadelphia, PA: WB Saunders Company; 2008.
- Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine. 1996;21(16):1889.
- Mens JM, et al. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine. 2002;27(2):196-200.
- Ostgaard HC, Zetherstrom G, Roos-Hansson E. The posterior pelvic pain provocation test in pregnant women. European Spine Journal. 1994;3:258-260
- Ozgocmen S, Bozgeyik Z, Kalcik M, Yildirim A. The value of sacroiliac pain provocation test in early active sacroiliitis. Clinical Rheumatology. 2008;10:1275-1282
- Potter N, Rothstein J. Intertester reliability for selected clinical tests of the sacroiliac joint. Physical Therapy. 1985;65:1671-1675
- Riddle D, Freburger J. Evaluation of the presence of sacroiliac joint dysfunction using a combination of tests: a multicenter intertester reliability study. Physical Therapy. 2002;82:772-781
- Robinson HS, Brox JI, Robinson R, et al. The reliability of selected motion & pain provocation tests for the sacroiliac joint. Manual Therapy. 2007;12:72-79
- Russell A, Maksymovich W, LeClerq S. Clinical examination of the sacroiliac joints. Arthritis Rheumatism. 1981;24:1575-1577
- Soleimanifar M, Noureddin K, Arab AM. Association between composites of selected motion palpation and pain provocation tests for sacroiliac joint disorders. Journal of Bodyworks and Movement Therapies. 2017;21:240-245
- Toussaint R, Gawlik C, Rehder U, Ruther W. Sacroiliac dysfunction in construction workers. Journal Manipulative Physiological Therapeutics. 1999;22:134-139
- van der Wurff P, Meyne W, Hagmeijer RH. Clinical tests of the sacroiliac joint-a systematic methodological review. Part 2-validity, Manual Therapy 2000;5(2):89-96
- Vincent-Smith B. Gibbons P. Inter-examiner & intra-examiner reliability of the standing flexion test. Manual Therapy. 1999;4:87-93
