Return to Sport
Return to Sport
How Do You Know When an Athlete is Really Ready?
Returning an athlete to sport is one of the most critical (and complex) decision in orthopedic and sports rehabilitation. Go too early, and you risk re-injury. Wait too long, and performance, confidence, or scholarship opportunities may suffer. So what is the solution? Use a comprehensive, evidence-based approach that includes physical, functional, and psychological readiness.
🔍 1. Beyond Time-Based Milestones
Historically, return-to-sport (RTS) decisions were made based on time from surgery or injury. For example, the “6-month rule” following ACL reconstruction is still widely cited. However, time alone is not a reliable predictor of tissue healing, neuromuscular recovery, or movement quality.
📌 Key Point: “Time from surgery should not be the sole determinant for return to sport.”
⚙️ 2. Functional Testing: Objective Readiness
Functional testing allows clinicians to assess whether the athlete can safely perform sport-specific movements with symmetry, strength, power, and control. The most commonly used return-to-sport tests include:
✅ Common Functional Tests:
-
Isokinetic Strength Testing (Quad and hamstring strength ≥90% of uninvolved side)
-
Hop Tests
-
Single hop for distance
-
Triple hop
-
Crossover hop

-
6-meter timed hop
-
Y-Balance Test (Anterior reach difference <4 cm between limbs)
-
Landing Error Scoring System (LESS) for biomechanical analysis
-
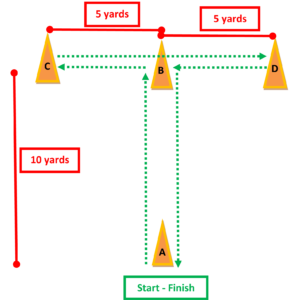
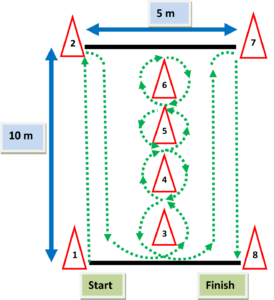
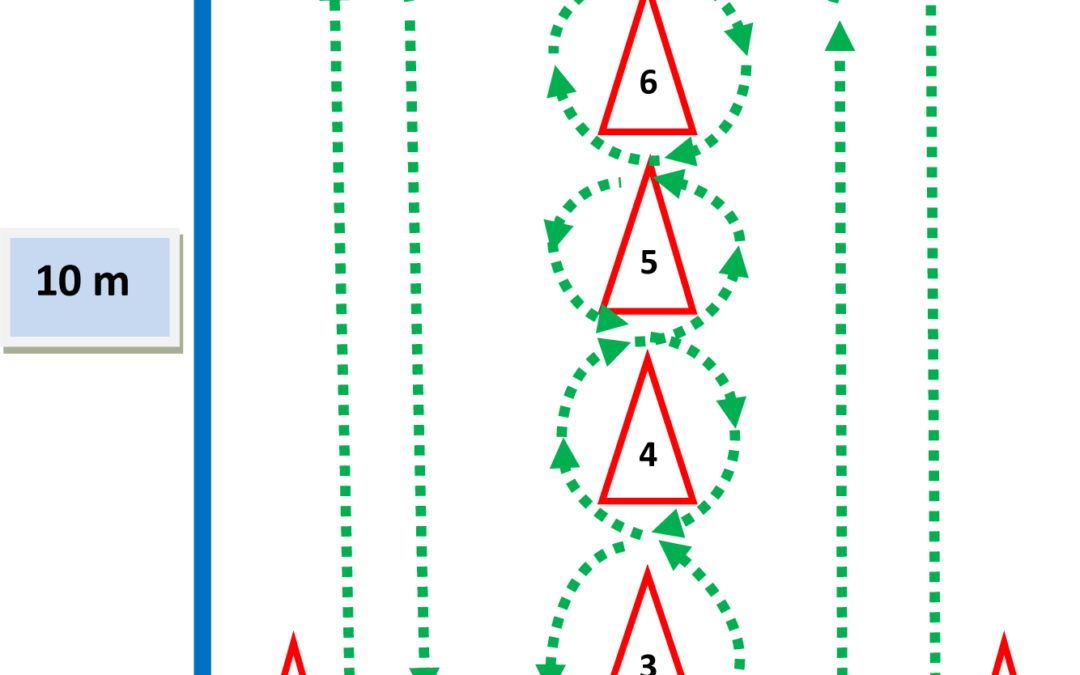
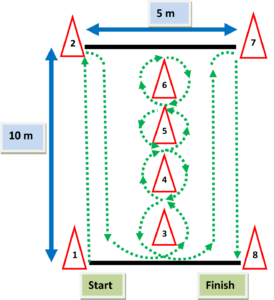
Agility & Sport-Specific Drills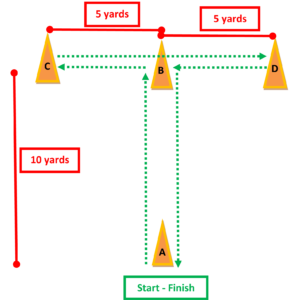
📌 Key Point: Athletes who fail to meet strength and hop symmetry benchmarks have 4x higher risk of ACL re-injury.
🧠 3. Psychological Readiness: The Missing Link
Even if an athlete passes physical tests, fear of re-injury, anxiety, or low confidence can prevent safe return to sport.
🧠 Validated Tools:
-
ACL-RSI (Return to Sport after Injury scale)
-
Measures confidence, emotions, and risk appraisal
-
Tampa Scale for Kinesiophobia (TSK)
-
https://www.carepatron.com/files/tampa-scale-for-kinesiophobia.pdf
-
Re-Injury Anxiety Inventory (RIAI)
-
https://pubmed.ncbi.nlm.nih.gov/20129120/
📌 Key Point: Athletes with low psychological readiness are significantly more likely to sustain a second injury or not return to sport at all.
🧩 4. Red Flags That Delay Return to Sport
-
Limb symmetry index <90% with the understanding the uninvolved extremity may have also experienced weakness during the injury and recovery time.
-
Poor landing mechanics (valgus, trunk lean)
-
Psychological hesitancy or high kinesiophobia
-
Pain, swelling, or instability with sport-specific movements
🧠 Conclusion: Return to Sport is Not a Date—It’s a Decision
Return to sport must be individualized, criterion-based, and multidisciplinary. Combining objective performance testing with psychological assessment gives athletes the best chance to return confidently—and safely.
For videos of all of these tests and more cutting edge orthopedic information iOrtho+ Premium Web App, please visit https://iortho.xyz/
Subscription is only $9.99/year or $1.99/month. All updates are FREE with an active subscription.
If you would like to learn more about the Mobil–Aider Orthopedic Arthrometer to quantify joint mobility, please visit: https://iortho.xyz/products/
-
Grindem H et al. (2016). “Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction.” British Journal of Sports Medicine, 50(13), 804–808.
-
Dingenen B, Gokeler A (2017). “Optimization of the return-to-sport paradigm after ACL reconstruction: a critical step back to move forward.” Sports Medicine, 47(8), 1487–1500.
-
Ardern CL et al. (2013). “A systematic review of the psychological factors associated with returning to sport following injury.” British Journal of Sports Medicine, 47(17), 1120–1126.
-
Shrier I et al. (2015). “Return to play following injury: whose decision is it, anyway?” British Journal of Sports Medicine, 49(7), 453–455.
-
Webster KE, Feller JA (2018). “Psychological readiness is associated with return to sport following ACL reconstruction.” Knee Surgery, Sports Traumatology, Arthroscopy, 26(7), 1981–1988.
-
Gulick DT (2025). iOrtho+ Premium Web App
 Return to Sport
Return to Sport