“Meniscal Injuries”
“Meniscal Injuries” 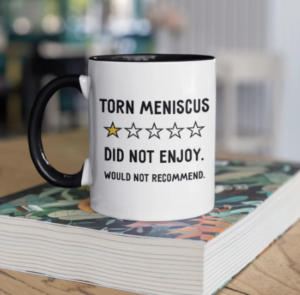
Meniscal Injury Mechanisms
There are several mechanisms of injury for a knee meniscus.
Healing of a meniscal injury has some challenges. Studies have shown that 10-30% of the periphery of the medial meniscus and 10-25% of the lateral meniscus has a vascular supply. The central region receives its nutrition from the synovial fluid from mechanical pumping and passive diffusion, a process known as imbibition. We know the vascular supply of the meniscus recedes as we age. In young children, more of the meniscus has a blood supply, so tears have a greater potential to heal. In adolescents and adults, about 80% of the meniscus has no blood supply, so tears in this inner meniscus are unlikely to heal.
Signs and symptoms of meniscal injuries may include:
- Joint line tenderness
- Swelling, popping, clicking, catching at joint line
- Lock in flexed position (bucket handle)
- Pain with flexion and weight bearing
- Presence of a Baker’s cyst
Meniscal Tests
There are about a dozen meniscal tests identified in the literature: some of the techniques for meniscal assessment are global and unable to distinguish the location of the tear, and others are more precise. Many of the metrics for the meniscal tests are highly variable because of the criteria used for a (+) test. Clicking, popping, snapping and/or pain could be deemed criteria for the presence of a meniscal injury.
Childress Duck Walking
For example, the Childress duck walking testis used to identify tears in the posterior horns of the meniscus because a deep squat compresses this region. However, there are other structures that could produce pain and limit the ability to perform a full squat. For these reasons, the statistical values of sensitivity (55-68%) and specificity (60-67%) are understandable.

 Ege Test
Ege Test
The Ege test adds hip internal (left) and external (right) rotation to the squat technique to increase the diagnostic parameters. Internal rotation is used to incriminate the lateral meniscus and external rotation the medial meniscus. The statistics support the addition of rotation to improve the specificity. 

 McMurray Test
McMurray Test
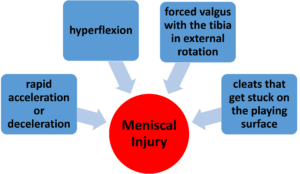
The McMurray test uses a combination of several motions to systemically incriminate the meniscus. This test takes both coordination and practice to perform it correctly. The patient is in a supine position. To assess the medial meniscus (left), the clinician uses one hand to grasp the distal tibia and places the other hand on the lateral aspect of the knee. Starting in full hip and knee flexion, the clinician passively extends the knee while imparting tibial ER and a valgus stress. To assess the lateral meniscus (right), the clinician uses one hand to grasp the distal tibia and the other places hand on the medial aspect of the knee. Starting in full hip and knee flexion, the clinician passively extends the knee while imparting tibial IR and a varus stress. Sometimes these maneuvers need to be performed a few times to “capture” the meniscus. A positive test would be clicking, snapping, or joint line pain. If the symptoms present with the knee in flexion, one might suspect a posterior meniscus injury, while symptoms in extension may be due to an anterior meniscus lesion. Statistics for this test are rather variable. Fortunately, when combined with the palpation of joint line tenderness, the metrics improve dramatically.
Joint line tenderness is just one other symptom that can be use in conjunction with the McMurray test to generate a Composite Score.

 Thessaly Test
Thessaly Test
The Thessaly test was first reported in the literature in 2005. Since that time, several studies have been published to validate the test for detecting meniscal tears (with and without anterior cruciate ligament lesions). This test is performed in weight bearing. With the clinician standing in front of the patient, hold on to the patient’s hands to assist balance. Ask the patient to stand on the uninvolved leg and flex the knee 5°. Now walk in an arc to one side of the patient, go back to center, and repeat in the other direction. The goal is to have the patient rotate on the knee while in a loaded/compressed status. Once the patient understands the motion, perform the test on the involved leg. The test is performed in both 5° and 20° of knee flexion. It is important to have the rotation occur through the legs not the trunk/shoulders. A positive test is clicking, locking, or catching of the meniscus.
An alternative is to have the patient uses the clinician’s shoulders for balance. The clinician places his/her hands on the patient’s hips and facilitates rotation with a compressive force. This confirms the transmission of a rotatory force through the knee. The Thessaly alone has strong diagnostic parameters but they improve just like the McMurray when joint line tenderness is also present.
Additional Tests
The Apley, Steinmann, and KKU tests are all very similar in technique to the Thessaly. They all simulate weight bearing via a longitudinal compression force through the tibia and incorporate a rotatory/shearing force. The Apley is performed in prone with the knee flexed to 90 degrees and a vertical compression force to the knee through the heel (left). Once compressed, the tibia is rotated medial and lateral. If a patient has a current ankle problem or a history of ankle instability, the test could be adapted to apply the rotation forces through the tibia. The Steinmann is performed in a supine position with the hip and knee in flexion. The knee is stabilized proximally and the thumb and index finger are used to palpate the knee joint line. The other hand grasps the tibia to apply an IR and ER force to the lower leg. This rotatory force is repeated in various knee positions (center). The KKU (named after a university in Thailand) was revealed in 2007. It is also performed in supine (right). The only difference between it and the Steinmann is that the KKU includes a compression force while rotating the tibia at 120°, 90°, 60°, 30°, and 0°. The statistics for these tests are summarized below.



In summary, there are a variety of meniscal tests with excellent literature to support their use. One should always listen to the patient’s history, understand the mechanism of injury, and reproduce their pain with at least two tests. For more cutting edge orthopedic information in iOrtho+ Premium Mobile App, please visit https://iortho.xyz/
- Akseki D, Ozcan O, Boya H, Pinar H. A new weight-bearing meniscal test & a comparison with McMurray & joint line tenderness. Arthroscopy. 2004;20:951-958
- Bhagia SM, Weinik M, Xing SY. Meniscal injury. eMedicine. June 30, 2009
- Boeree NR, Ackroyd CE. Assessment of the meniscus & cruciate ligaments: an audit of clinical practice. Injury. 1991;22(4):291-294
- Corea JR, Moussa M, al Othman A. McMurray’s test tested. Knee Surgery Sports Traumatology Arthroscopy. 1994;2:70-72
- Evans PJ, Bell GD, Frank C: Prospective evaluation of the McMurray test, American Journal Sports Medicine 1993;21:604-608
- Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy. 1989;5:184-186
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC. 2020
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia. 2018
- Harrison BK, Abell BE, Gibson TW. The Thessaly test for detection of meniscal tears: validation of a new physical examination technique for primary care medicine. Clinical Journal of Sports Medicine. 2009;19:9-12
- Hegedus EJ, Cook C, Hasselblad V, et al. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. Journal of Orthopedic Sports Physical Therapy. 2007;37:541-550
- Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN. Diagnostic Accuracy of a New Clinical Test (The Thessaly Test) for Early Detection of Meniscal Tears. Journal of Bone & Joint Surgery. May 2005;87A(5):955-962
- Kim SJ, Min BH, Han DY: Paradoxical phenomena of the McMurray test: an arthroscopic examination, American Journal Sports Medicine. 1996;24:83-87
- Konan S, Rayan F, Haddad FS. Do physical diagnostic tests accurately detect meniscal tears? Knee Surgery Sports Traumatologic Arthroscopy. 2009;17(7):806-811
- McMurray TP: The semilunar cartilages, British Journal Surgery 1942;29:407-414
- Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal injury. Clinical Rehabilitation, 2008;22:143-161
- Mirzatolooei F, Yekta Z, Bayazidchi M, Ershadi S, Afshar A. Validation of the Thessaly test for detecting meniscal tears in anterior cruciate deficient knees. The Knee. 2010;17(3):221-223
- Pookarnjanamorakot C, Korsantirat T, Woratanarat P. Meniscal lesions in the anterior cruciate insufficient knee: the accuracy of clinical evaluation. Journal Medical Association of Thailand. 2004;87:618-623
- Sae-Jung S, Jirarattanaphochai K, Benjasil T. KKU knee compression-rotation test for detection of meniscal tears: a comparative study of its diagnostic accuracy with McMurray test. Journal Medical Association of Thailand. 2007;90(4):718-723
- Shelbourne KD, Martini DJ, McCarrell JR et al: Correlation of joint line tenderness and meniscal lesions in patients with acute anterior cruciate ligament tears, American Journal Sports Medicine 1995;23:166-169
- Snoeker BAM, Lindeboom R, Zwinderman AH, Vincken PWJ, Jansen JA, Lucas C. Detecting meniscal tears in primary care: Reproducibility and accuracy of 2 weight-bearing and 1 non-weight-bearing tests. 2015
- Stratford PW, Binkley J. A review of the McMurray test: Definition, interpretation, & clinical usefulness. Journal Orthopedics Sports Physical Therapy. 1995;22(3):116-120