

The Patella – More than Just a Sesamoid Bone
Although the patellofemoral joint is not a true articulation, is serves a very important purpose. As the largest sesamoid bone in the body, it forms the least congruent joint in the body. The patella is stabilized by transverse and longitudinal restraints. The transverse restraints are the medial and lateral retinacula which joins the vastus medialis and lateralis, respectively. The longitudinal restraints are the quadriceps and patellar tendons. The patella lengthens the moment arm by increasing the distance of the quadriceps and patellar tendon from the axis of the knee. Acting as a pulley, the patella changes the line of pull of the muscle and reduces the friction between the quad tendon and the femoral condyles.
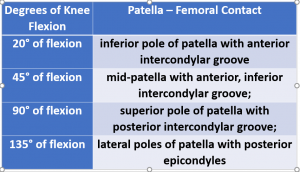
In knee extension, the patella is suspended over the femur-tibia articulation. In full extension, there is no contact between the patella and the femoral sulcus beneath it. This is because the quad tendon pulls from superior & the patellar tendon pulls from inferior. As the knee moves into flexion, contact of the patella with the femoral condyles begins inferiorly and shifts superior and lateral. This occurs as the pull of the quad/patellar tendons become oblique. At ~90°, the patella is in contact with both condyles but beyond 90°, the patella rotates (67°) laterally so that only the medial condyle articulates with the patella. In full flexion the patella slides distally on the femoral condyles (7-8 cm of vertical movement) and sinks into the intercondylar notch. Failure of the patella to slide, tilt, and/or rotate will result in decreased ROM, pain, and/or destruction of the patellofemoral surfaces.
One of the measures frequently taken of the patella is the Q-angle: a measurement from the anterior superior iliac spine (ASIS) to mid-patella to tibial tubercle (measured in knee extension). A normal Q-angle is 17° ± 3° in females and 14° ± 3° in males. However, this is a static measure and cannot be changed. Some would say the measure is of no clinical value.
Dynamic Q-angle is a much more functional measure. Willson and Davis (2008) and Philips (2006) looked at what happens with people who have patellofemoral pain when descending stairs. They found the Q-angle of a person without patellafemoral pain was 24° versus 39° in a person with patellofemoral syndrome. This significant increase in Q-angle is believed to be related to a very poor level of hip control. The femur was not being controlled eccentrically when going down the stairs. As previously stated, this theory was supported by literature that demonstrated the importance of hip strength for knee function. Predictive values have been reported to be hip ER strength is less than or equal to 20.3% of body weight and hip abduction strength is less than or equal to 35.4% of body weight (Khayambashi, Ghoddosi, Straub, & Powers, 2016).
Assessing mobility of the patella is another technique to evaluate the patella-femoral joint. However, sitting with the knee in extension, quadriceps relaxed, and translating the patella superior/inferior, medial/lateral, and tilting has not been deemed very reliable. These maneuvers are difficult to quantify and normative data has not been established. The ability to assess diminished or absent patellar mobility is as follows: 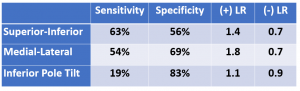
The Helfet test is used to assess patella alignment in the frontal plane. When sitting or supine with the knee flexed to 90°, the tibial tuberosity should be in line with midline of the patella. When the knee is extended, the tibial tuberosity should be in line with the lateral border of the patella. Inappropriate alignment of the patella can impact the tracking during movement and result in dysfunction.
Fairbank apprehension and moving patella apprehension tests assess patella mobility relative to the tendency to subluxate/dislocate. Both tests are very similar but as the tests imply, one is static and the other dynamic. The Fairbank apprehension test (static) is performed in supine with the quadriceps relaxed and the knee flexed to 30°. The clinician pushes the patella distal and lateral. For the moving patella apprehension test (dynamic) the patient is sitting and the clinician uses his/her thumb to translate the patella laterally. This lateral pressure is maintained as the knee is flexed to 90° and back to full extension. A positive test is apprehension of the patient or contraction of quadriceps to prevent lateral displacement of patella. Hence the title of the tests: apprehension tests. 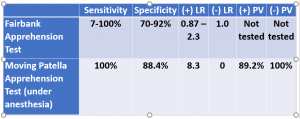
Another patella test is the Active Patella Grind Test. As the name of the test implies, it is a very uncomfortable test and really fails to provide any clinical value. Not only does the test not have any statistical data, this test is painful even for people with no patellofemoral dysfunction. It is performed by having the patient sit with knee flexed to 90° and the clinician places the cupped hand over the superior edge of the patient’s patella. The patient SLOWLY extends the knee. The location of the crepitis and/or pain (degrees of flexion) is stated to correspond with the contact of the various patella and femoral surfaces.
Collectively, the available patella mobility tests have limited value in assessing dysfunction. The most valuable assessment is the dynamic valgus (Q-angle) measure because it is the one measurement you influence. The use of hip strengthening exercises can externally rotate the femur under the patella as opposed to trying to move the patella medially on the femur.
For more cutting edge orthopedic information in iOrtho+ Premium Mobile App, please visit the learning modules at https://iortho.xyz/
- Ahmed CS, McCarthy M, Gomez JA, Shubin Stein BE. The moving patellar apprehension test for lateral patellar instability. American Journal Sports Medicine. 2009;37(4):791-796.
- Fairbank HAT: Internal derangement of the knee in children and adolescents, Proceedings Review Society Medicine 1937;30:427-432
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia 2018
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC 2020
- Haim A, Yaniv M, Dekel S, Amir H. Patellofemoral pain syndrome: validity of clinical & radiological features. Clinical Orthopedics. 2006;451: 223-228
- Helfet A: Disorders of the knee, Philadelphia, JB Lippincott. 1997
- Hughston JC, Walsh WM, Puddu G: Patellar Subluxation & Dislocation, Philadelphia, WB Saunders. 1984
- Khayambashi K, Ghoddosi N, Straub RK, Powers CM. Hip Muscle Strength Predicts Noncontact Anterior Cruciate Ligament Injury in Male and Female Athletes: A Prospective Study. American Journal of Sports Medicine. 2015 Dec 8. epub
- Kim SJ, Lee DH, Kim TE. The relationship between the MPP test & arthroscopically found medial patellar plica pathology. 2007;23(12):1303-1308
- Magee D. Orthopedic Physical Assessment. 5th ed. Philadelphia, PA: WB Saunders Company; 2008.
- Nijs J, Van Geel C, Van der auwera D, Van de Velde B. Diagnostic value of five clinical tests in patellofemoral pain syndrome. Manual Therapy. 2006;11:69-77
- Niskanen RO, Paavilainen PJ, Jaakkola M, Korkala OL. Poor correlation of clinical signs with patellar cartilaginous changes. Arthroscopy. 2001;17:307-310
- Reider B: The orthopedic physical examination, Philadelphia, 1999, WB Saunders.
- Sweitzer BA, Cook C, Steadman JR, Hawkins RJ, Wyland OJ. The inter-rater reliability & diagnostic accuracy of patellar mobility tests in patients with anterior knee pain. Physician & Sports Medicine. 2010;3(38):90-96
- Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical Biomechanics. 2008;23(2):203-211
