

Shoulder Mobilizations: Does Direction Matter?
Shoulder Biomechanics
Let’s start with the anatomic structure of the shoulder. The humeral head is convex and the glenoid fossa is concave. So, the convex-concave rule indicates the movement of convex on concave result in rolling and gliding of joint surfaces in opposite directions. While concave on convex result in rolling and gliding in the same direction. What does that mean? When elevating the shoulder, the convex humeral head will roll superior and glide inferior in the glenoid fossa. Well, that is sort of true but not quite that simple. Work done by Matsuli et al (2012) in vivo, looked at the kinematics of elevation in the scapular plane. The study revealed a 2.1 mm superior translation of the humeral head in the glenoid from 0 to 105° of elevation and 0.9 mm of inferior glide from 105° to endrange. Although there is an inferior glide with elevation, the net result is a slightly more superior humeral head by endrange elevation. This can be significantly influenced by the strength/weakness of the rotator cuff musculature but that is beyond the scope of this blog.
Let’s explore the actual mechanics of shoulder mobilizations and the related literature. The shoulder is one of the most mobile joints of our bodies. The chart below summarizes the arthrokinetic motions for each respective osteokinematic movement: 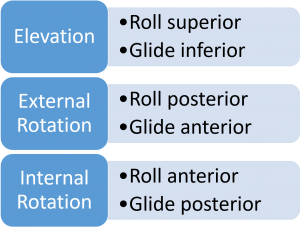
Inferior Glide
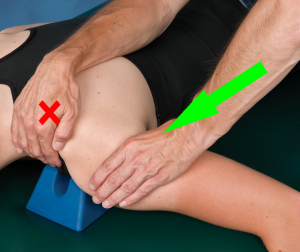
To perform an inferior glide to improve elevation, the clinician drapes his/her hand with a towel or pillow case. The patient rests in the supine position with the involved upper extremity (UE) over the edge of the plinth. The clinician places the web-space of the draped hand in the axilla for stabilization (X). Note the posterior border of the clinician’s forearm presses against the patient’s rib cage to enhance stability. The other hand grasps the distal humerus to impart an inferior glide of the humerus on the glenoid socket. Note the parallel alignment of the clinician’s lateral arm and the patent’s humerus (Wise & Gulick, 2009).
 This technique can also be performed from a superior position. One would stand at the head of the patient with the involved UE supported on the plinth. By palpating the joint space of the shoulder, one can move lateral to identify the humeral head. The clinician places the web-space of the hand on the superior aspect of the humeral head and aligns his/her forearm in the direction of desired force. This technique can also be quantified by using the Mobil–Aider device. To do this, the green attachment (H-E) is donned in the custom dovetail slot. The device is lined up with the joint line and an inferior force is directed through the superior humeral head. The reading on the device screen appears in millimeters of movement. If the device is in the “A” mode, the maximal reading will be held for several seconds for ease of reading. If in the “B” mode, the reading is a real-time measure to permit consistency of the joint mobilization in the range of the desired grade. For example, if the total excursion of the humerus is 8 mm, the clinician would want to do oscillations to 5-8 mm for a grade III and 7-8 mm for a grade IV mobilization. In conjunction with the Mobil–Aider reading, one could determine if the arthrokinematic motion improved and the corresponding impact on the osteokinematic measurement (Gulick, 2020).
This technique can also be performed from a superior position. One would stand at the head of the patient with the involved UE supported on the plinth. By palpating the joint space of the shoulder, one can move lateral to identify the humeral head. The clinician places the web-space of the hand on the superior aspect of the humeral head and aligns his/her forearm in the direction of desired force. This technique can also be quantified by using the Mobil–Aider device. To do this, the green attachment (H-E) is donned in the custom dovetail slot. The device is lined up with the joint line and an inferior force is directed through the superior humeral head. The reading on the device screen appears in millimeters of movement. If the device is in the “A” mode, the maximal reading will be held for several seconds for ease of reading. If in the “B” mode, the reading is a real-time measure to permit consistency of the joint mobilization in the range of the desired grade. For example, if the total excursion of the humerus is 8 mm, the clinician would want to do oscillations to 5-8 mm for a grade III and 7-8 mm for a grade IV mobilization. In conjunction with the Mobil–Aider reading, one could determine if the arthrokinematic motion improved and the corresponding impact on the osteokinematic measurement (Gulick, 2020).
A study by Bang and Deyle (2000) examined the influence of inferior glides on individuals with shoulder impingement. They divided the patients into two groups: exercise and exercise with manual therapy. They all received 6 treatments over three weeks. The manual therapy included inferior glides of the shoulder and this group had a greater improvement in pain, strength, and function than the exercise group alone. A study by Delgado-Gil et al (2015) reported similar results with patients with impingement.
Shoulder Rotation
Joint mobilizations to facilitate shoulder rotation have been classically been identified as anterior glides for external rotation (ER) and posterior glides for internal rotation (IR). However, it may not be that simple. In many individuals with poor posture and shoulder pathology, the humeral head is not centered in the glenoid fossa. If the humeral head is too anterior, there is not enough anterior glide to permit full ER. This lack of anterior glide will then limit ER. By performing a posterior glide to center the humeral head, this will restore the needed anterior translation for ER (Wise & Gulick, 2009). Now let’s look at how these techniques are performed.
Posterior Glide
To perform a posterior glenohumeral glide, the patient should be supine. The clinician’s hand is underneath the scapula to create some space for the translation of the humeral head. You can also achieve this spacing with a wedge or a towel as well. The distal humerus (elbow) should also be supported on a towel and the hand draped across the abdomen. As you know, the humeral head is not at a 90-degree angle in the sagittal plane. Thus, a posterior glide needs to be angled posterior-lateral in order to avoid having the posterior glenoid rim stop the glide. To do this, the clinician places the thenar eminence on the anterior humeral head and directs the forearm in a posterior-lateral direction.
 When the Mobil–Aider is used for a posterior glide, the blue (H-D) attachment is donned. The joint line is identified, the device is aligned with the joint line and the same technique is performed. The magnitude of the posterior oscillations can be observed on the screen to discern the linear translation performed relative to the total translation, i.e. grade of mobilization.
When the Mobil–Aider is used for a posterior glide, the blue (H-D) attachment is donned. The joint line is identified, the device is aligned with the joint line and the same technique is performed. The magnitude of the posterior oscillations can be observed on the screen to discern the linear translation performed relative to the total translation, i.e. grade of mobilization.
Anterior Glide
 To perform an anterior glenohumeral glide, the patient is positioned in prone. A wedge/towel roll should be place under the anterior chest/clavicle, medial to the glenohumeral joint line. This lifts the chest off the plinth and permits room to glide the humerus anterior. The scapula is stabilized proximally (X) and the web space of the clinician’s hand contacts the humeral head to perform an anterior medial glide (Hint: Remember orientation of the humerus in the glenoid fossa). Once again, one needs to attend to the alignment of the forearm relative to the desired motion. The same positioning and technique using the Mobil–Aider is
To perform an anterior glenohumeral glide, the patient is positioned in prone. A wedge/towel roll should be place under the anterior chest/clavicle, medial to the glenohumeral joint line. This lifts the chest off the plinth and permits room to glide the humerus anterior. The scapula is stabilized proximally (X) and the web space of the clinician’s hand contacts the humeral head to perform an anterior medial glide (Hint: Remember orientation of the humerus in the glenoid fossa). Once again, one needs to attend to the alignment of the forearm relative to the desired motion. The same positioning and technique using the Mobil–Aider is  displayed to the right.
displayed to the right.
Several studies have demonstrated the efficacy of anterior/posterior glides of the shoulder. Celik et al (2016) performed distractions, inferior, anterior, and posterior glides on individuals with adhesive capsulitis. Each technique was performed at 2-3 oscillations/sec, 2-3 minutes each, and 3-4x each. During weeks 1 – 2, grades I and II joint mobilizations were performed. During weeks 3 – 6, grade III and IV joint mobilizations were performed. After 18 treatments, joint mobilization combined with stretching exercises were better than stretching exercise alone in terms of external rotation, abduction range of motion and function score. This was consistent with the results of Teys, Bisset, and Vicenzino (2008) who had significant improvement over sham and control conditions with posterior-lateral glides. Vermeulen et al (2006) also studied the effects of inferior, anterior, and posterior glides on adhesive capsulitis. However, they compared grades I and II to grades II and IV. Although both groups demonstrated marked improvement in shoulder range of motion, shoulder Rating Questionnaire, Shoulder Disability Index, SF-36, and VAS, the higher grade mobilizations were significantly better. Finally, to demonstrate the importance of centering the humeral head in the glenoid fossa, Johnson (2007) compared the influence of anterior to posterior glides to increase shoulder ER. After six treatments, the individuals receiving posterior glides demonstrated 15 degrees more ER than the anterior glide group.
In summary, direction does matter! It is important to know the shoulder anatomy and kinematics but it is critical to assess the position of the humeral head to appreciate the appropriate direction of mobilization.
To download iOrtho+ Premium Mobile App, please visit: https://iortho.xyz/
For more information on the Mobil–Aider and joint mobilization techniques, please visit the learning modules at https://mobil-aider.com
- Bang MD, Deyle GD. Comparison of supervised exercise with and without physical therapy for patients with shoulder impingement syndrome. JOSPT. 2000;30(3):126-137
- Celik D, Mutlu EK. Does adding mobilization to stretching improve outcomes for people with frozen shoulder? A randomized controlled clinical trial. Clinical Rehabilitation. 2016;30(8):786-94.
- Delgado-Gil JA, Prado-Robles E, Rodrigues-de-Souza DP, Cleland JA, Fernandez-de-las-Penas C, Alburquerque-Sendin F. Effects of mobilization with movement on pain and range of motion in patients with unilateral shoulder impingement syndrome: A randomized controlled trial. Journal of Manipulative Physiologic Therapy. 2015;38(4):245-52.
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC, 2020
- Johnson AJ, Godges JJ, Zimmerman GJ, Ounanian LL. Effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. JOSPT. 2007;37(3):88-99.
- Matsuki K, et al. Dynamic In vivo glenohumeral kinematics during scapular plane abduction in healthy shoulders. JOSPT. 2012;42(2):96-104
- Teys P, Bisset L, Vicenzino B. Initial effects of a Mulligan’s mobilization with movement technique on range of movement and pressure pain threshold in pain-limited shoulders. Manual Therapy. 2008;13(1):37-42.
- Wise CH, Gulick DT. Mobilization Notes. FA Davis Publishing, Philadelphia, 2009
- Vermeulen HM, Rozing PM, Oberman WR, le Cessie S, Vliet Vlieland TPM. Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: Randomized controlled trial. Physical Therapy. 2006;86(3):355-368
